Retinal Detachment
There are three types of retinal detachments. The most common form is where a break in the retina’s sensory layer causing fluid to seep underneath. This eventually causes a separation in the layers of the retina. Individuals who are particularly short sighted, with historic eye injuries or who have undergone eye surgery are most susceptible to this type of detachment. This is due to the thinner and more fragile retina in short sighted people. The second most common type is due to increased traction on the retina by strands of scar or vitreous tissue which can ultimately pull the retina loose.
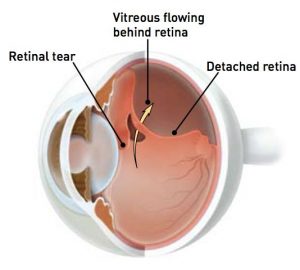 The third most common type occurs when small pockets of liquid form within a special gel (the vitreous) which usually lines the inside of the eye. Eventually, some of this fluid moves in between the gel and the retina, causing the vitreous to peel away from the retina. The retina, which is like the film of a camera, is then able to see the outer part of this gel floating inside the eye – and this is what causes floaters. Sometimes, when the vitreous gel comes away from the retina, it can pull on the retina, causing a hole or tear to appear in the retina. This is because the vitreous gel sometimes has areas where it is strongly attached to the retina. As the gel falls away from the retina (a bit like wall-paper falling from the wall), the gel can tear the retina (like the wallpaper may take a piece of paint or plaster from the wall).
The third most common type occurs when small pockets of liquid form within a special gel (the vitreous) which usually lines the inside of the eye. Eventually, some of this fluid moves in between the gel and the retina, causing the vitreous to peel away from the retina. The retina, which is like the film of a camera, is then able to see the outer part of this gel floating inside the eye – and this is what causes floaters. Sometimes, when the vitreous gel comes away from the retina, it can pull on the retina, causing a hole or tear to appear in the retina. This is because the vitreous gel sometimes has areas where it is strongly attached to the retina. As the gel falls away from the retina (a bit like wall-paper falling from the wall), the gel can tear the retina (like the wallpaper may take a piece of paint or plaster from the wall).
If a hole or tear develops in the retina, then there is an increased risk of there being a full retinal detachment. A detached retina will cause loss of vision, and requires surgical intervention to put the retina back in the right place. Thus, it is very important that you have your eye examined urgently on the onset of any symptoms. There are other less common reasons for floaters – e.g. bleeding into the gel in the back of the eye from a blood vessel (usually in diabetic patients).